HIV Lens data methods
HIV Lens allows users to search HIV data by age, exposure group, age and geographic region, where available. Data have been produced by the UK Health Security Agency and all information presented is in the public domain as official statistics or published reports.
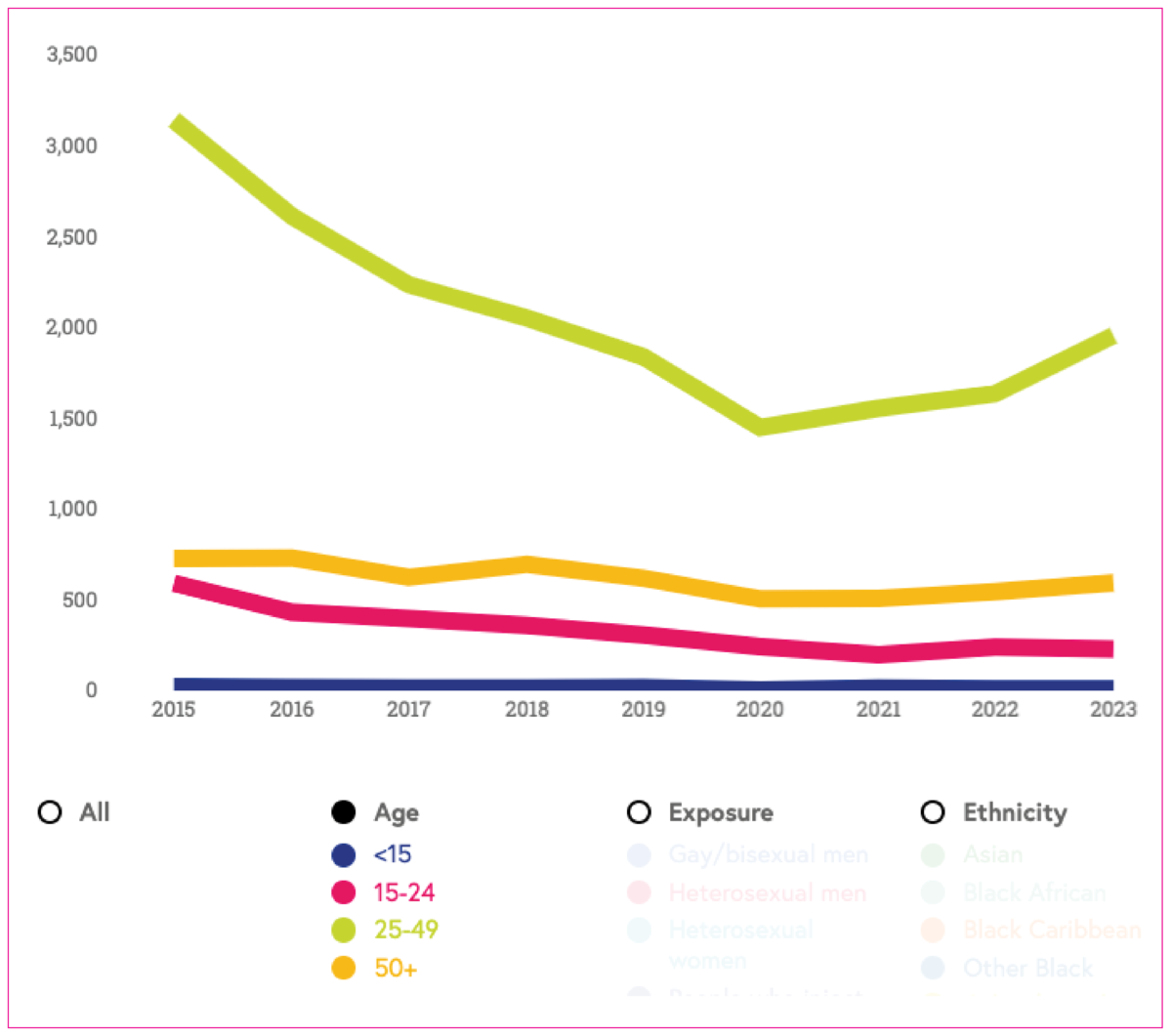
Number of new HIV diagnoses first made in England
HIV diagnoses among people with no previous diagnoses abroad reported.
All new HIV diagnoses
The data show all new HIV diagnoses.
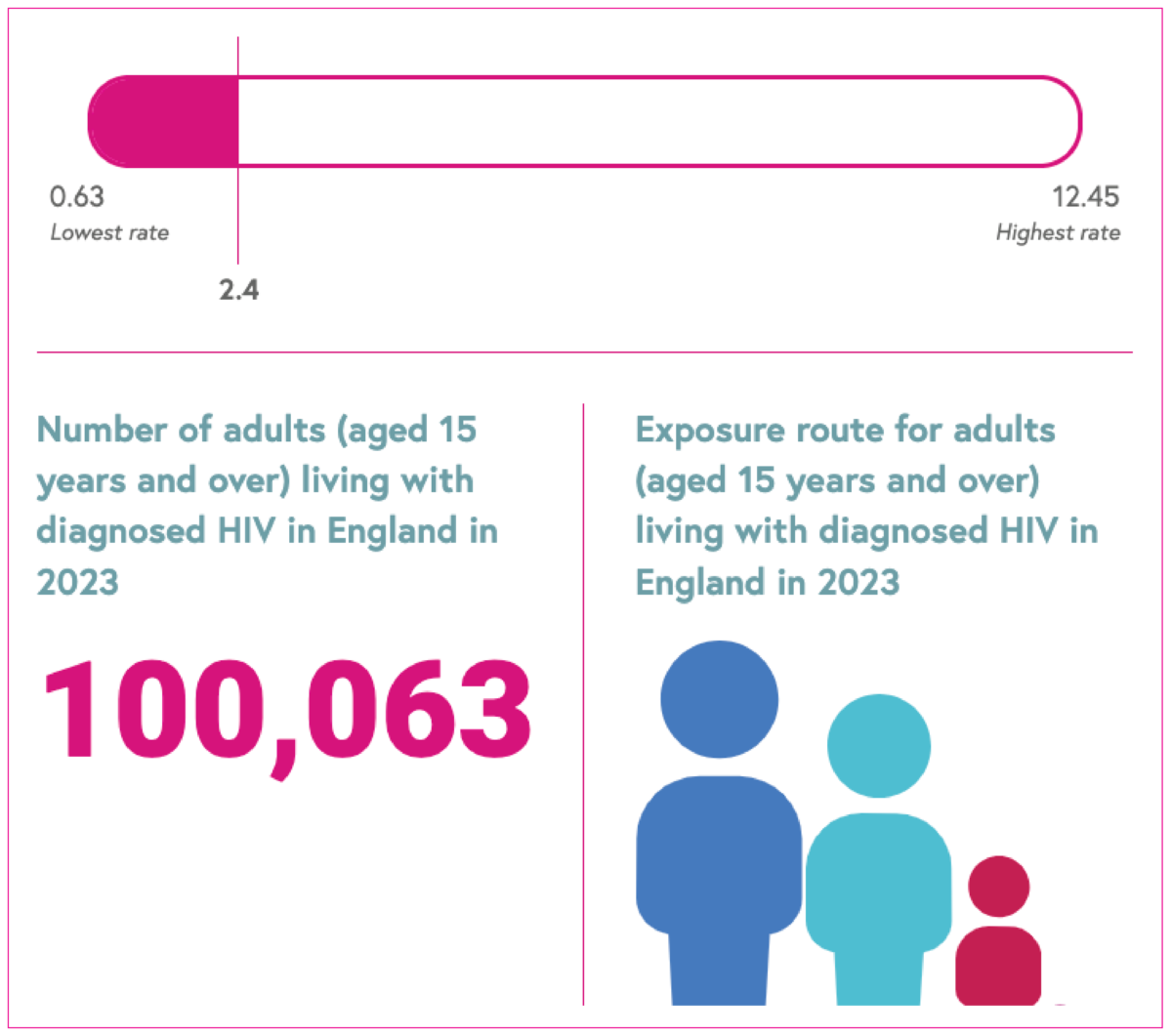
Living with diagnosed HIV
The rate of people living with diagnosed HIV per 1,000 people aged 15-59 years, and the number of adults aged 15 years and over.
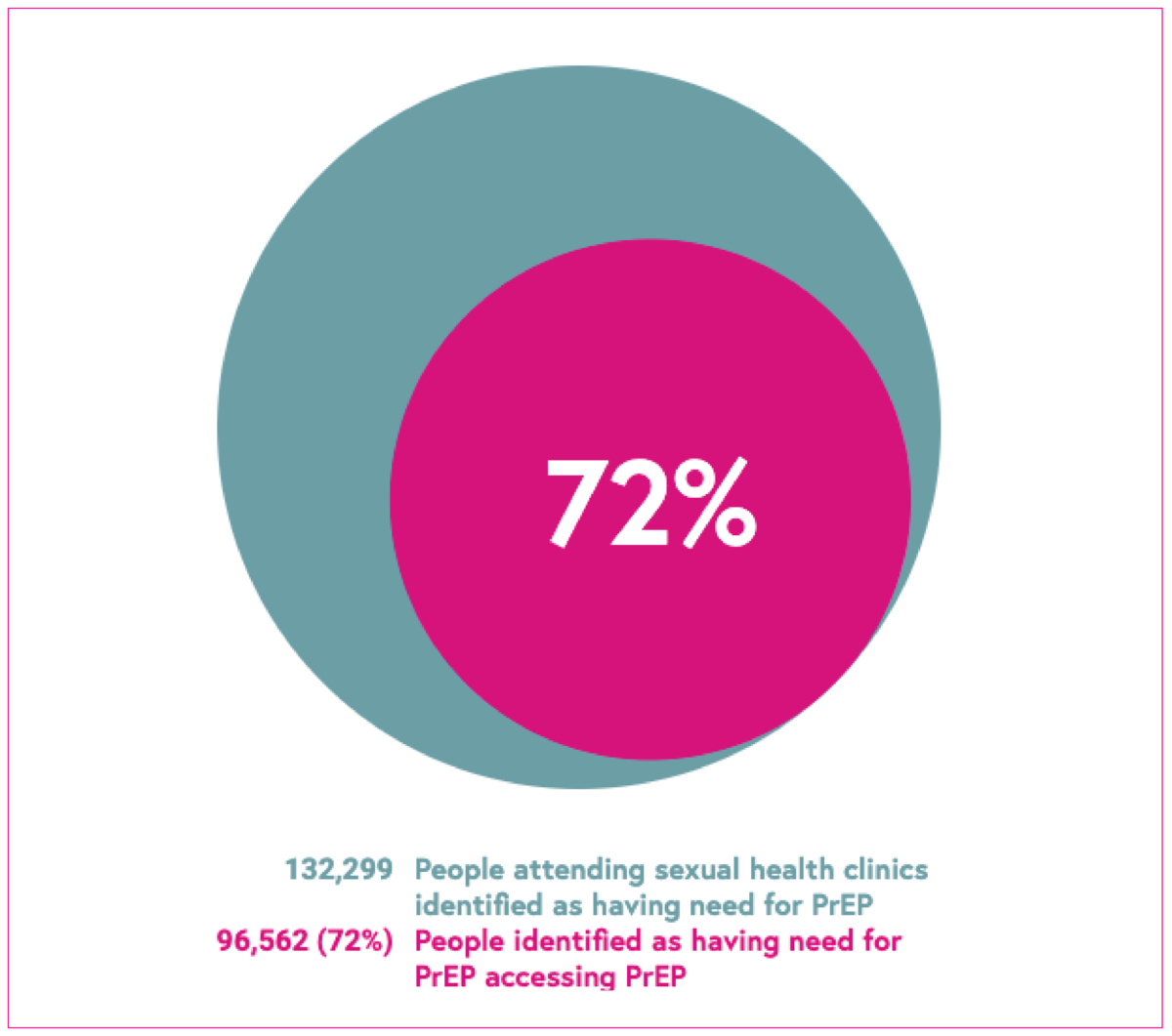
PrEP
This indicator shows the number of people attending sexual health services identified as having need for PrEP, and the proportion accessing PrEP.
HIV testing rate
This measure shows the proportion of people living in a specific area who had an HIV test at a sexual health clinic.
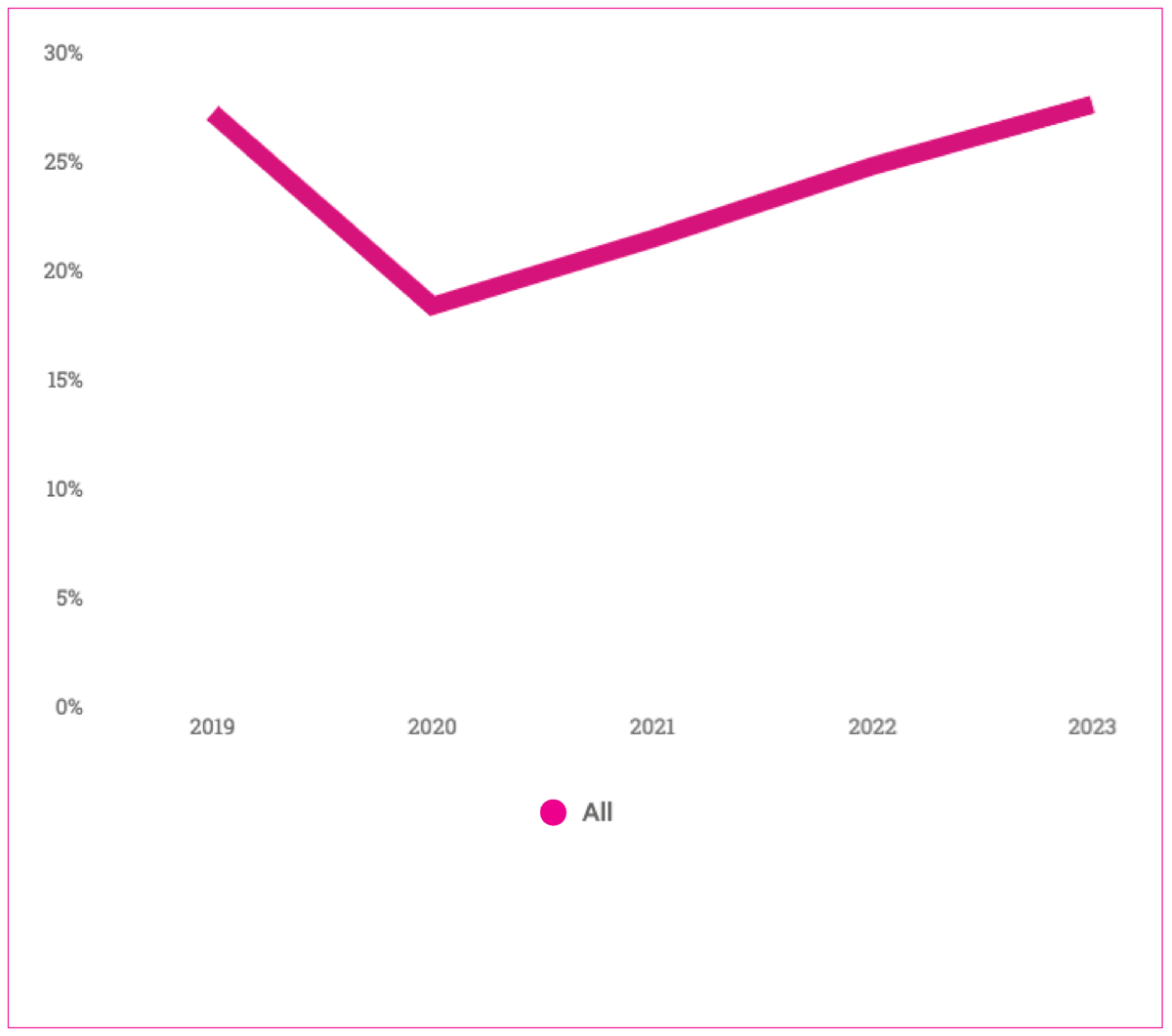
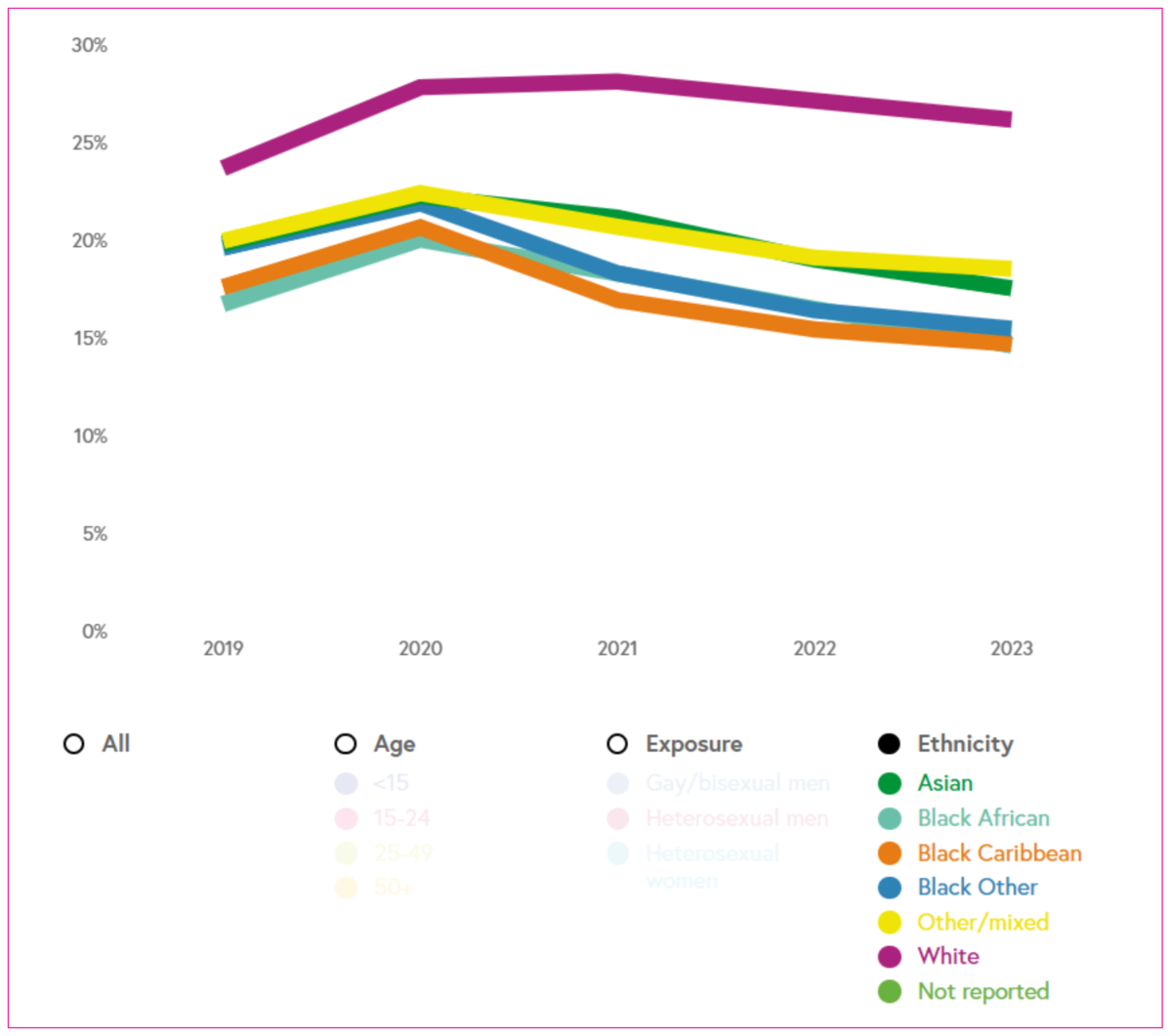
Proportion of people declining a test
The proportion of people attending a sexual health service who were offered, but declined, an HIV test.
Emergency department testing
The proportion of people attending an emergency department who have blood taken who have an HIV test; who test positive; and who were newly diagnosed with HIV.
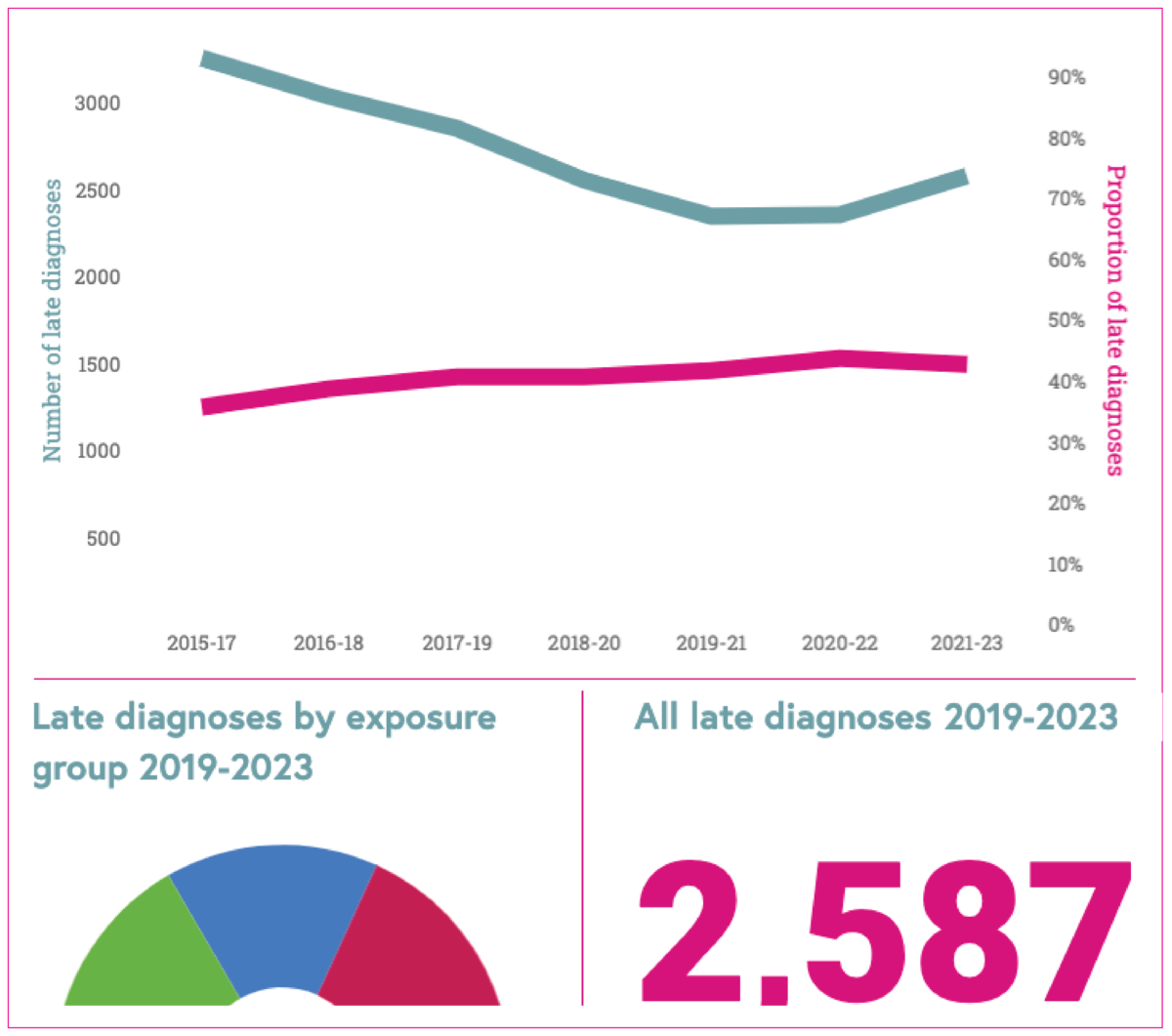
Late diagnoses
The number and proportion of HIV diagnoses made at a late stage of infection.
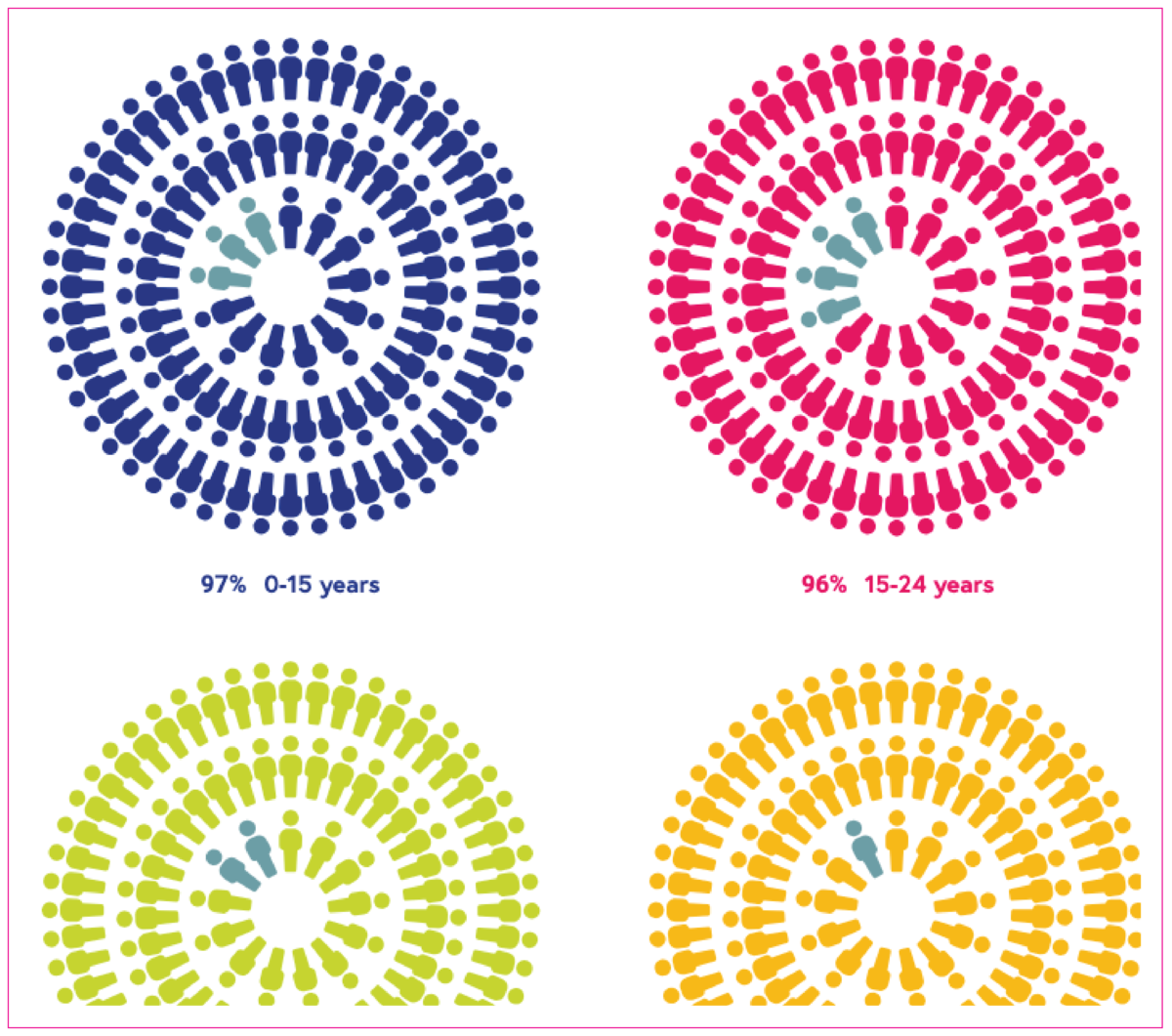
Treatment started within 91 days
The proportion of people who started treatment within 91 days of HIV diagnosis.
HIV treatment coverage
The percentage of people with diagnosed HIV receiving HIV treatment.
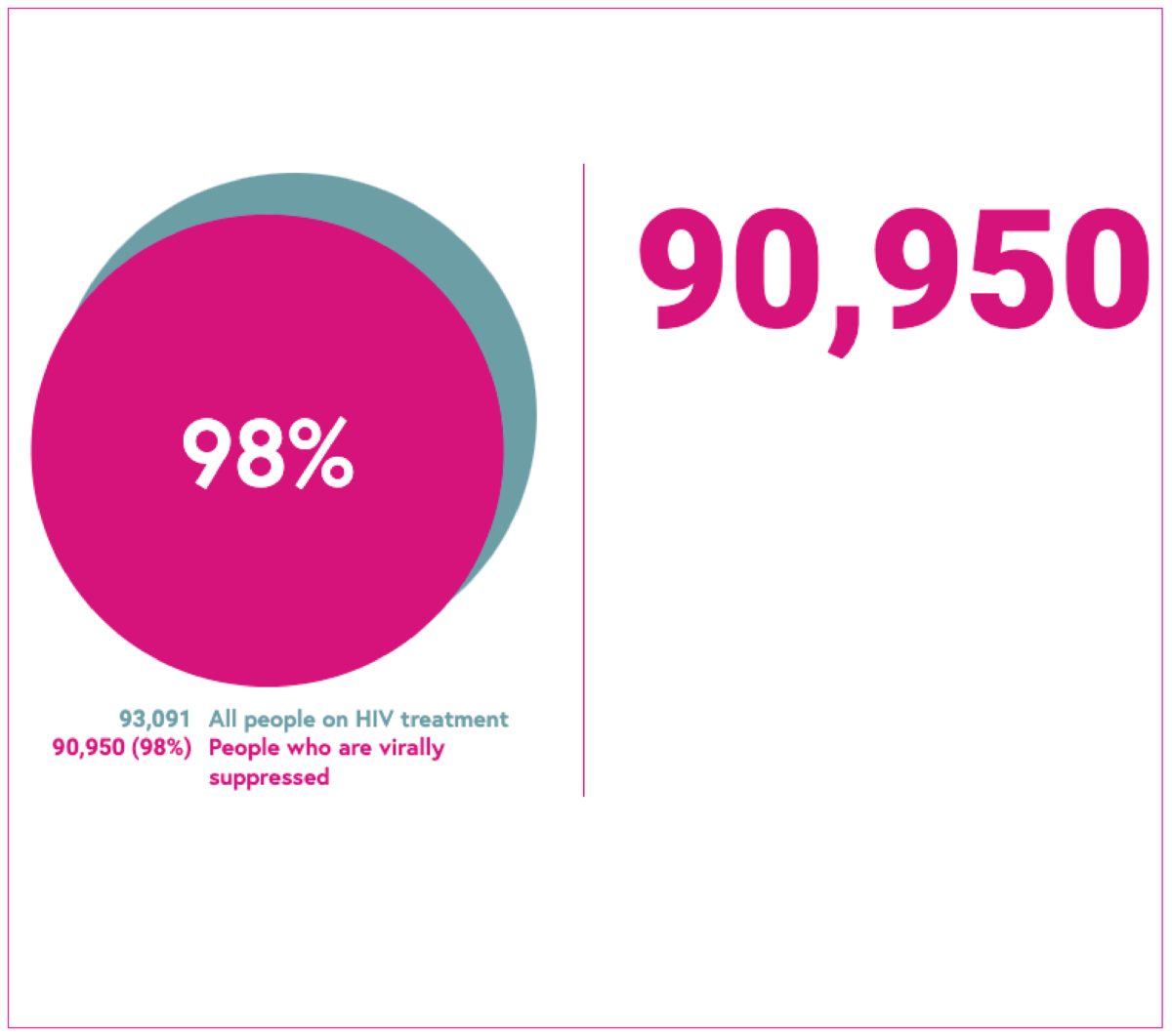
Viral suppression
Proportion of people with diagnosed HIV receiving treatment who are virally suppressed.
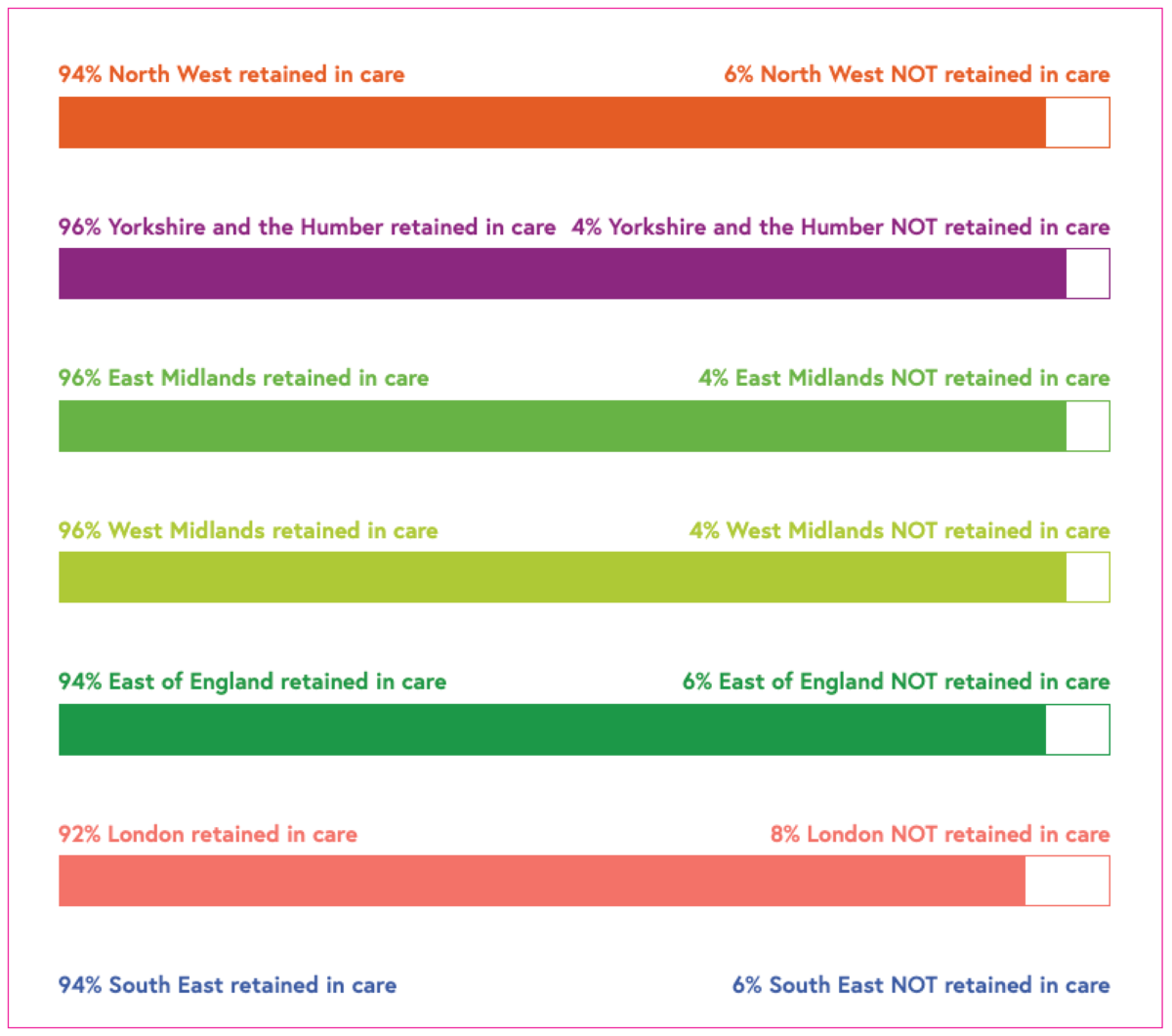
Retention in care
The proportion of people seen for HIV care who are seen on an annual basis.
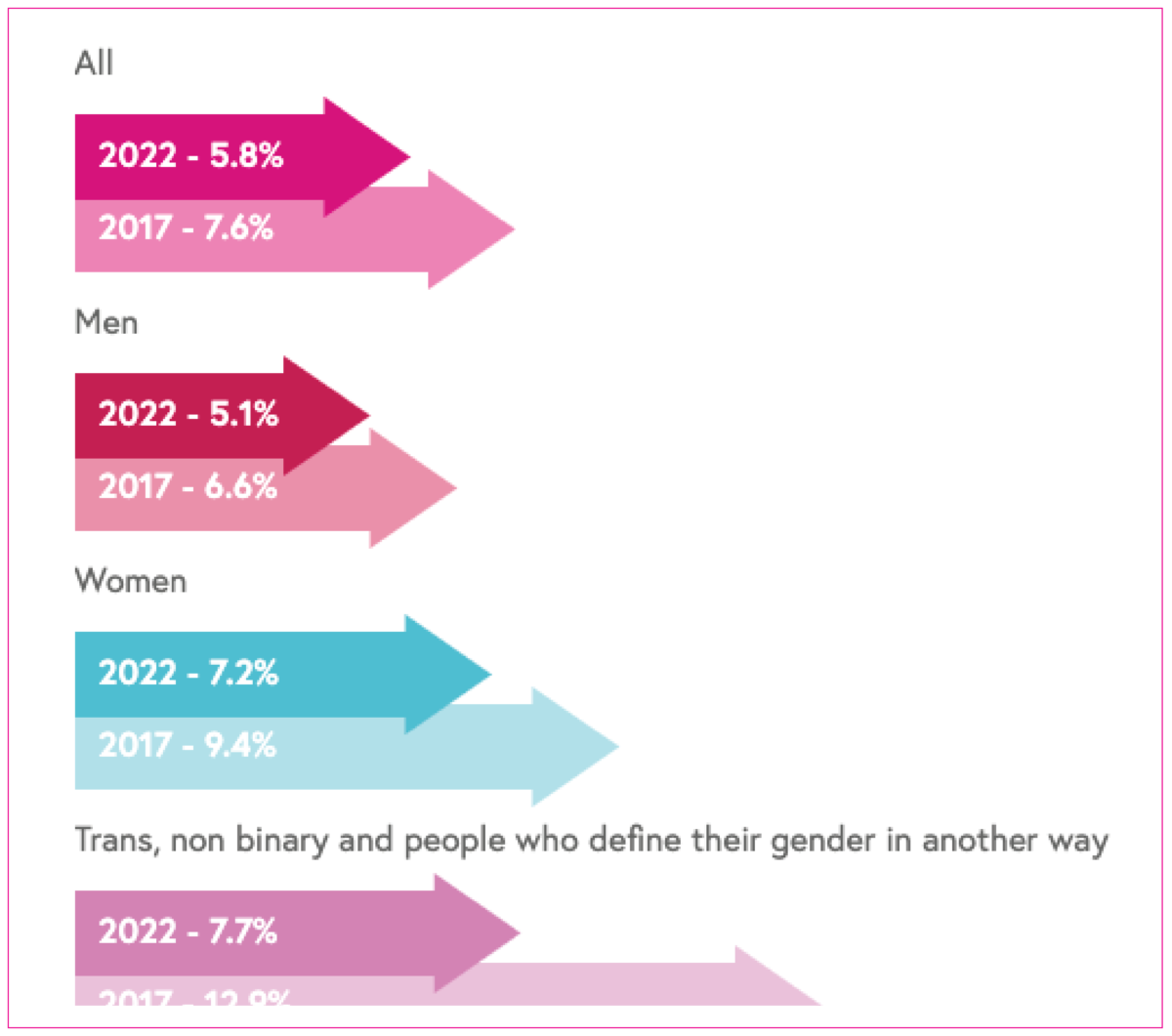
HIV stigma
Data from the Positive Voices survey on stigma in healthcare settings, anticipated stigma, and sharing one’s HIV status.
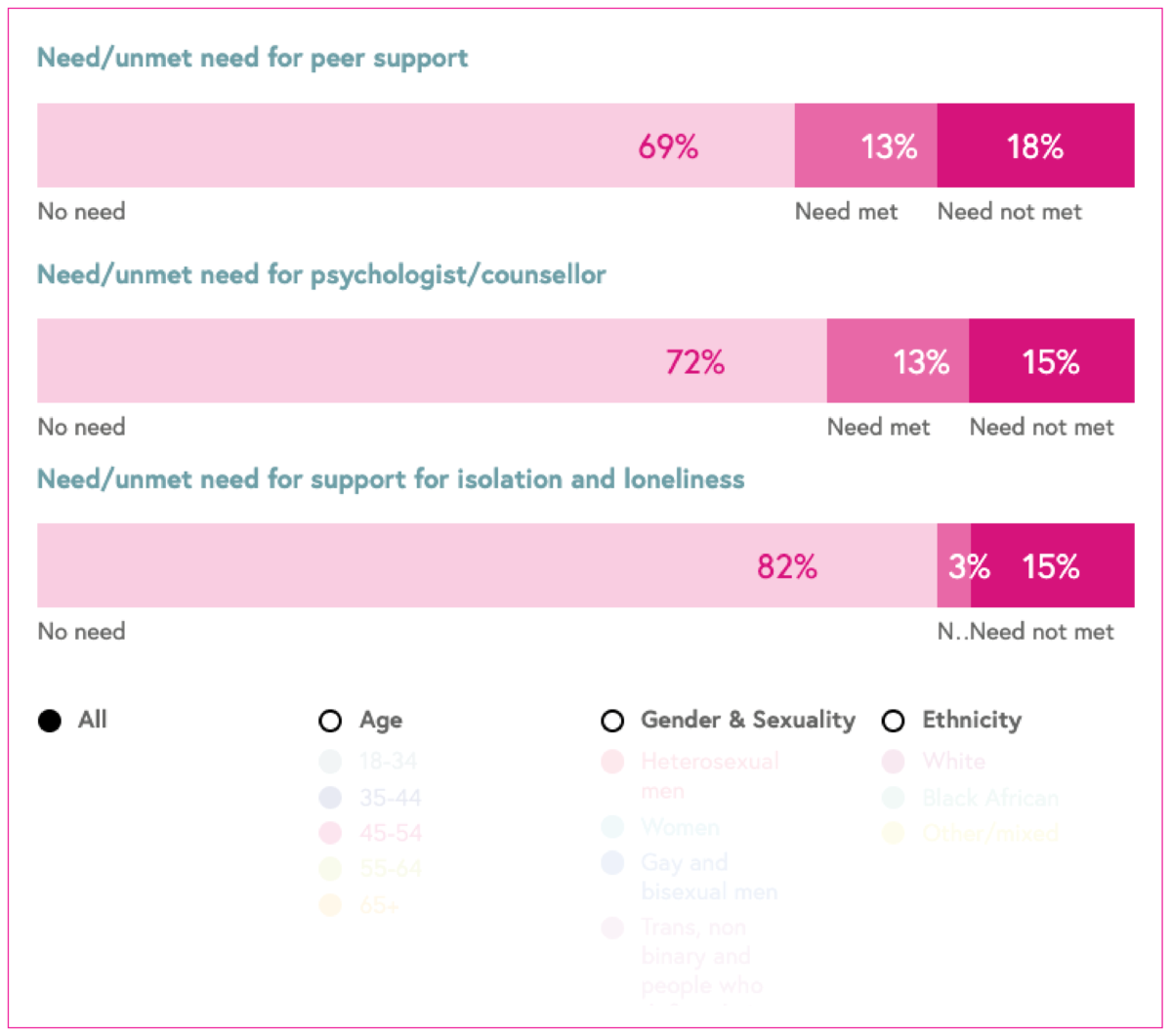
Needs of people living with HIV
Data from the Positive Voices survey on the 'need' and 'unmet need' for services of people living with HIV.
Indicator
Definition
Number of new HIV diagnoses first made in England
New HIV diagnoses first made in England are used as proxy for HIV transmission in the HIV Action Plan. This is because it excludes HIV probably acquired abroad. New diagnoses must be interpreted together with trends in HIV testing. The HIV Action Plan aims to reduce new HIV diagnoses first made in England by 80% between 2019 and 2025. If new HIV diagnoses decrease at the same time as HIV testing rises or stays the same, this indicates a fall in transmission.
Breakdown: age, exposure, ethnicity (where available), and geographic region.
All new HIV diagnoses
All HIV diagnoses include people continuing HIV care in the UK, who were diagnosed with HIV abroad. Consequently, all HIV diagnoses do not represent transmission. We use new HIV diagnoses first made in England as a proxy for transmission. However, people can live with undiagnosed HIV infection for many years. This means that new HIV diagnoses are not necessarily infections that have been recently acquired. These data must be interpreted together with trends in HIV testing.
Breakdown: age, exposure, ethnicity (where available), and geographic region of diagnosis.
Living with diagnosed HIV
The rate of people living with a diagnosed HIV infection per 1,000 people aged 15-59 years is used to inform HIV testing guidelines.
Rates are categorised as follows:
- Extremely high >5 per 1,000
- High 2-5 per 1,000
- Low <2 per 1,000.
In areas with high and extremely high HIV prevalence, HIV testing services should be expanded outside of sexual health settings in accordance with NICE and BHIVA testing guidelines.
We also show as a number the total number of adults (15 years and over) living with diagnosed HIV infection.
Breakdown: exposure (where available) and geographic region.
PrEP
Pre-exposure prophylaxis (PrEP) is a drug taken by HIV-negative people prior to sex to stop HIV acquisition. As part of a combination approach to HIV prevention, the roll out of routine PrEP commissioning began in England in the autumn of 2020. Specialist sexual health services (SHS) are responsible for the delivery of PrEP to those at higher risk of acquiring HIV.
Two indicators are presented.
Determining PrEP need. This indicator is used to determine PrEP need among people accessing specialist SHS. It assesses the proportion of all HIV-negative people accessing specialist SHS who are at substantial HIV risk, and therefore could benefit from receiving PrEP. This shows which populations are in highest need of PrEP.
Initiation or continuation of PrEP among those with PrEP need. This indicator assesses what proportion of individuals accessing specialist SHS with PrEP need start or continue PrEP. The higher the proportion, the better PrEP need is being met through providing PrEP.
Breakdown: geographic region.
HIV testing rate
This measure shows the proportion of people living in a specific area who had an HIV test at a sexual health clinic.
Breakdown: geographic region (where available).
Proportion of people declining a test
The proportion of people declining a test shows the proportion of people attending a sexual health service who were offered, but declined an HIV test.
Breakdown: age, exposure, ethnicity and geographic region (where available).
Emergency department testing
These data are from the UKHSA 24 month evaluation report of the NHSE programme to implement opt out BBV testing in emergency departments in high HIV prevalence settings. Only HIV information is presented here.
Three indicators are presented, which use a subset of 16 of the 33 clinics involved in the opt out programme. Most of the clinics are based in London with clinics in Sussex, Manchester and Blackpool also included in the programme.
The first indicator measures the proportion of people attending 16 of 33 emergency department who have blood taken as part of their care, who have an HIV test.
The second indicator measures the proportion of people who had an HIV test in 16 of 33 clinics who tested positive (including known HIV infections as well as newly diagnosed infections).
The third indicator measures the proportion of people who had an HIV test who were newly diagnosed with HIV from the 16 of the 33 clinics.
Late diagnoses
Adults (aged 15 years and over) only. The data measure the proportion and number of HIV diagnoses that are made with CD4 counts <350 cells within 91 days of diagnosis, which is indicative of a late stage of infection. The lower the proportion, the better.
A person diagnosed late has been living with an undiagnosed HIV infection for around three to five years and is more susceptible to infections compared to a person with a higher CD4 count. People diagnosed late have a tenfold increased risk of death compared to those diagnosed promptly.
People with a CD4 count <350 who have evidence of recently acquired HIV infection have been excluded.
Data are presented for three years combined.
Breakdown: exposure (where available), and geographic region of diagnosis.
Treatment started within 91 days
This indicator presents the number and proportion of people newly diagnosed with HIV who start antiretroviral therapy within 91 days of their diagnosis. HIV treatment saves lives and prevents onward HIV transmission.
Data is presented by area of residence and exclude people diagnosed with HIV in England who are resident in Wales, Scotland, Northern Ireland or abroad.
Breakdown: geographic region (where available).
HIV treatment coverage
The number of people taking antiretroviral treatment at their last clinic attendance divided by everybody in HIV care. HIV treatment saves lives and prevents onward HIV transmission. The higher the proportion, the better.
Breakdown: age, exposure, ethnicity (where available), and geographic region.
Viral suppression
A viral load under 200 copies/ml. The number of people who are virally suppressed (<200 copies/ml) divided by the number of people receiving HIV treatment. A person who has suppressed virus at this level is unable to pass on HIV infection to sexual partners. This is known as Undetectable = Untransmittable (U=U). The higher the proportion, the better.
Breakdown: geographic region.
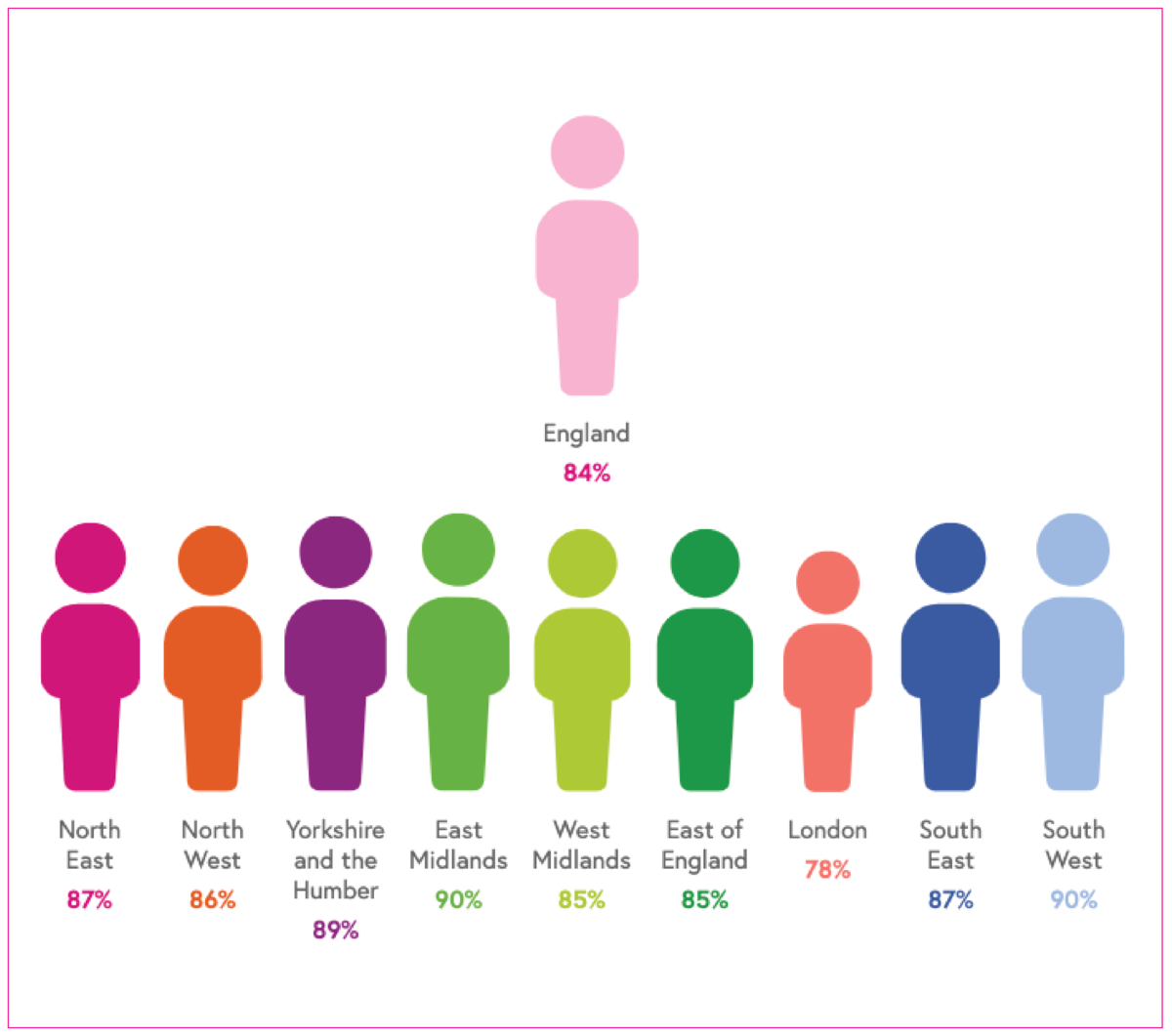
Retention in care
This indicator measures the extent people seen for HIV care are seen on an annual basis, in accordance with BHIVA standards of care. People in care have their HIV monitored to ensure good health, the right medication and to assess whether they are virally undetectable. The retention in care measure assesses the proportion of people seen within 15 months of their last attendance date up to and including October 2021. The higher the proportion, the better.
Breakdown: geographic region (where available).
HIV stigma
Data is from the Positive Voices survey. This is a representative survey conducted in 2017 and 2022 of people living with HIV who provided information about their lived experience in relation to satisfaction with HIV care, treatment, co-morbidities, lifestyle, needs and unmet needs and stigma.
The questions asked about stigma related to life satisfaction, enacted stigma in healthcare settings (experiences of being treated badly), anticipated stigma (avoiding health care because of HIV stigma) and sharing one’s HIV status.
Breakdown: gender.
Needs of people living with HIV
Data relating to need is from the 2022 Positive Voices survey. Positive Voices was a representative survey conducted in 2017 and 2022 of people living with HIV who provided information about their lived experience in relation to satisfaction with HIV care, treatment, co-morbidities, lifestyle, needs and unmet needs and stigma.
The proportion of ‘need’ was defined as the percentage of people with HIV who stated their need for a service, out of all those who responded to the question. The proportion of ‘unmet need’ was defined as the percentage of people with HIV who did not receive it, out of those who stated they needed the service.
Breakdown: age, gender and sexuality, and ethnicity.